 Spring, 2015
Spring, 2015
Lung surfactant is a material that lines the air-sacs in the lungs and is essential for breathing. Premature babies are often born before they have a chance to produce sufficient lung surfactant and they need to be given surfactant in order to help them breathe. This surfactant is generally sourced from animals.
People of any age who are seriously ill or injured also frequently have damage to their lung surfactant, which impairs their ability to breathe. One such condition, called Acute Respiratory Distress Syndrome (ARDS), affects 150,000 people per year in the US, and has a fatality rate of about 40%. Unlike with premature babies, treating adults with surfactant derived from animals has been very challenging for two reasons. First, adult lungs are larger than a baby’s and it’s therefore difficult to get enough animal surfactant together to cover it. Second, there are hostile conditions present in the lungs of ARDS patients that deactivated their own lung surfactant, and that rapidly inhibits surfactant.
Dr. Valerie Booth is working with a multi-disciplinary team at Memorial University and a research team in Spain to understand the essential features of the proteins in natural lung surfactant and to use this knowledge to develop artificial lung surfactant treatments that are more resistant to deactivation.
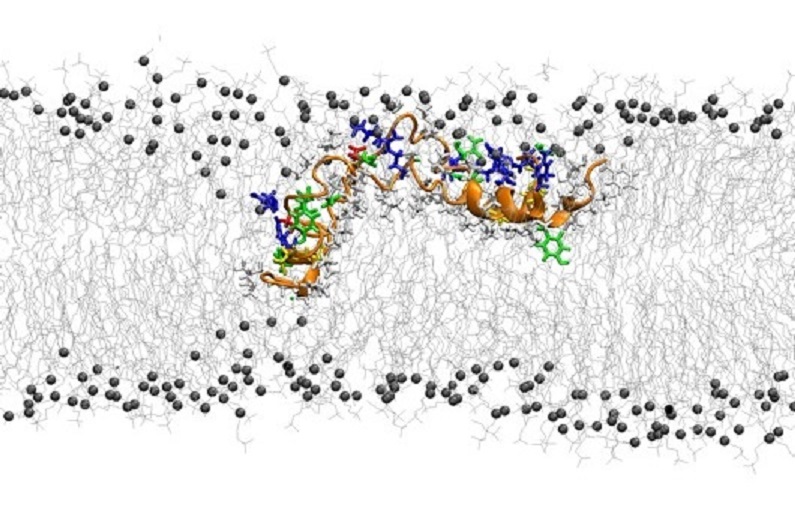
Specifically, Booth’s research focuses on Surfactant Protein B (SP-B). SP-B is of particular importance because unlike the other lung surfactant proteins, you absolutely can’t live without it in your lungs. Furthermore, unlike most essential proteins, we strangely do not know the three-dimensional structure of SP-B, or what it looks like. Consequently, we don’t understand how it works. This is because SP-B is exceptionally hard to work with experimentally.
SP-B is very hydrophobic, a fancy word for sticky. It likes to stick to greasy, lipid molecules instead of to water. Despite the challenges, it is possible to use experimental techniques to find out small pieces of information about its structure. However, the key to unlocking SP-B’s molecular structure is through running simulations on Compute Canada infrastructure. Booth’s group uses these simulations to make predictions about what SP-B looks like, and then compares those to the experimental data in order to provide the best possible picture of SP-B.
Proteins are like tiny molecular machines and we can’t figure out how they work until we know what they look like. Determining what SP-B looks like tells researchers how it works. Understanding how we breathe will help Booth develop a treatment for ARDS. In fact, she, two of her PhD students and a research assistant are currently working towards a provisional patent for a formulation for artificial surfactant, with the hope it will result in an industrial partnership.
Illustration courtesy of Mohammad Hassan Khatami